Fecal calprotectin, promising the future!
Inflammatory bowel disease (IBD) is a chronic inflammatory bowel disease that mainly involves the digestive system, and Crohn's disease (CD) and ulcerative colitis (UC) are the main types of it. Common complications of UC include toxic megacolon, colonic stenosis, intestinal obstruction, intestinal bleeding, intestinal perforation, colon polyps, and colon cancer; common complications of CD include fistula, abdominal abscess, intestinal obstruction, and perianal lesions, less likely to develop into a cancer.
Inflammatory bowel disease is an inflammatory reaction caused by the abnormal response of the intestinal mucosal immune system under the interaction of multiple factors such as environment, genetics, infection, and immunity. Compared with common enteritis, its characteristic is that the state of an illness shows effect repeatedly, protractedly. Once a patient gets this kind of disease , it will cost him a lot of money on diagnosis and treatment.
Clinically, the diagnosis and evaluation of inflammatory bowel disease include intestinal endoscopy, imaging examination, laboratory blood test, and clinical activity index score, etc. which are invasive, with disadvantages such as radioactivity, high cost, time-consuming, and poor compliance. In contrast, fecal calprotectin (FC) detection has the advantage of solid practicability, simple and convenient operation, repeatable detection, low cost, and less time-consuming, which just meet the clinical needs. FC serves as an excellent biomarker for diagnosis and prognostic assessment.
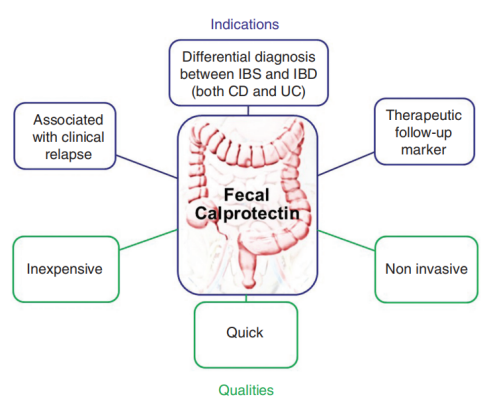
Figure 1: Indications and main advantages of calprotectin in clinical practice
Image credit: Manceau H, Chicha-Cattoir V, Puy H, Peoc'h K. Fecal calprotectin in inflammatory bowel diseases: update and perspectives. Clin Chem Lab Med.
FC can specifically reflect intestinal inflammation
Calprotectin is a calcium-zinc-binding protein with a relative molecular mass of 36 kD. It is an inflammatory marker, mainly derived from neutrophils, and a small amount derived from monocytes and macrophages. When intestinal inflammation occurs, neutrophils infiltrate and release calprotectin due to the increased permeability of intestinal mucosa, which can be detected in feces. Therefore, FC is closely related to intestinal inflammation. Due to the combination with calcium ions, it is highly stable in feces, which is superior to previous fecal markers.
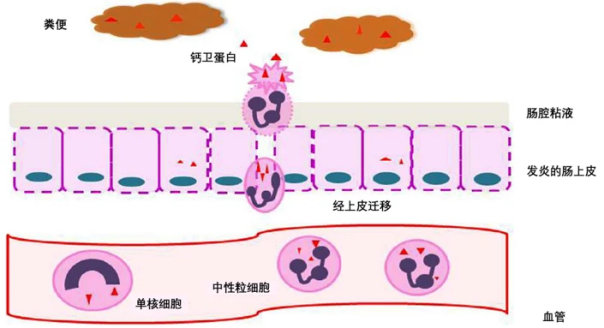
Figure 2: Mechanisms by which FC reflects intestinal inflammation
Image source: Manceau H, et al. Clin Chem Lab Med. 2017 Mar 1;55(4):474-483.
Van Rheene et al conducted a meta-analysis that included 13 studies with a total of 1041 IBD patients, and found that the sensitivity and specificity of FC in the differential diagnosis of adults and children with IBD were 93%, 96%, 96%, and 76%, respectively.
FC levels correlate with disease activity in inflammatory bowel disease
The study shows that when a 50ug/g FC level is used as a threshold, the sensitivity and specificity are 89% and 58% respectively, and when at 70ug/g FC level, the sensitivity and specificity are 89% and 72%. Another prospective study involving 100 patients with IBD suggested that sensitivity and specificity in diagnosing UC activity with thresholds of 50ug/g and 102ug/g were 85% and 79%, while sensitivity in patients with CD with thresholds of 54ug/g and 122ug/g was the same (71%). Specificity was different (63% vs 71%). According to the above studies, we find the FC threshold directly affects its ability to discriminate disease activity, which greatly affects the clinical application of FC. Therefore, based on previous research results, clinicians proposed a demarcation standard: when FC concentration is <50 ~ 100ug/g, the disease is considered to be in remission; when FC concentration is between 100 ~ 250ug/g, the disease may be active and further examination is required. when FC concentration is >250ug/g, the disease is considered to be active.
Assess the efficacy of drug therapy
Guidi et al conducted a study involving 62 IBD patients to monitor the therapeutic response of FC to anti-TNF preparations and found that the level of FC in patients who responded to treatment was lower than that of patients who did not respond to treatment, and when the cut-off value was 168g, the sensitivity was 83%, with a specificity of 74%.
Predict disease recurrence
A prospective study included 163 patients and found that relapsed patients had higher FC levels and FL positive rates, and the ability of FC to predict recurrence was stronger than that of FL. Mao et al conducted a meta-analysis that included 6 studies with a total of 672 IBD patients and found that the sensitivity and specificity of FC in predicting disease recurrence were 78% and 73%, respectively, and its ability was no difference to predict recurrence among patients. In addition, FC can also be used to predict postoperative recurrence in IBD patients. A study from Australia found that FC>100ug/g had a sensitivity of 89% in predicting endoscopic recurrence, and its predictive ability was significantly higher than other clinical indicators such as CRP. Orlando et al. detected the concentration of FC in 39 CD patients 3 months after intestinal resection and found that when the cut-off value was 200ug/g, the sensitivity of predicting postoperative recurrence was 63%, and the specificity was 75%.

Summarize
Fecal calprotectin has a very important value and status in the diagnosis and treatment of inflammatory bowel disease. Fecal calprotectin can better reflect the degree of intestinal inflammation, monitor disease activity, evaluate the efficacy of drug treatment, and predict disease recurrence.
References
[1] "Consensus of Patients with Inflammatory Bowel Disease"
[2] Xiong Yangyang, Wang Jinrong, Li Binchao, Fu Yu, Zhang Yalin, Kong Juan. New progress in research on inflammatory bowel disease. Journal of Medical Research, 2015, 44(7): 168-170.
[3] Fan Xing, Weng Xiechuan, Ding Rigao. Research progress on etiology of inflammatory bowel disease. International Journal of Digestive Diseases, 2013(1):6-8.
[4] Wu Weirong, Xia Zhongsheng, Zhuang Yanyan, Zhong Yingqiang, Zhong Wa. Current status of diagnosis and treatment of small bowel adenocarcinoma associated with Crohn's disease. Guangdong Medicine, 2022, 43(10): 1312-1316.
[5] Zhang Lijuan, Sun Baiyang, Li Hui. Application value and progress of endoscopic ultrasonography in the diagnosis and treatment of inflammatory bowel disease. Modern Digestive and Interventional Diagnosis and Treatment, 2020, 25(12): 1676-1680.
[6] Shen Jia, Xie Fang. The detection method of fecal calprotectin and its research progress in inflammatory bowel disease. Big Doctor, 2023, 8(5): 141-144.
[7]Manceau H, Chicha-Cattoir V, Puy H, Peoc'h K. Fecal calprotectin in inflammatory bowel diseases: update and perspectives. Clin Chem Lab Med. 2017 Mar 1;55(4):474-483. doi: 10.1515/cclm-2016-0522. PMID: 27658156.
[8]Manceau H, et al. Clin Chem Lab Med. 2017 Mar 1;55(4):474-483.
[9] Xie Haohao, Wu Xiuwen, Wang Junjun. Application of biomarkers related to inflammatory bowel disease. Chinese Journal of Laboratory Medicine, 2018, 41(10): 716-719.




